- +1.888.528.8757
- office@doctorspreferredhhc.com
- Monday – Friday 9 AM – 5 PM
For people over the age of 55-60, macular degeneration of the retina is one of the leading causes of permanent loss of central vision. The degeneration of the macula – the most important part of the retina responsible for the level of central objective vision required for visual work, reading text at close range, or driving vehicles – is the cause of the loss of visual functions, while peripheral vision in such patients is usually unaffected.
The condition causes the patient to lose objective eyesight, suffer a drop in overall performance, and become disabled, all of which contribute to the disease’s significant socio-medical relevance. At the same time, depending on the type of age-related macular degeneration and the severity of the illness, macular degeneration of the retina of the eye can cause both a slowly progressive loss of vision and a sudden loss of eyesight in a matter of months.


Let’s traverse through the anatomy of the photosensitive section of the eyeball – the retina – to comprehend the substance of the diseased process. The retina is made up of two layers and is placed at the rear of the visual organ. The inner layer is made up of rods and cones, which are photosensitive cells. These cells function as receptors, responding to light signals that reach the retina of the eye and transmitting information to the optic nerve. Cones aid in the recognition of things in daylight and in the formation of color vision. In turn, the sticks are in charge of twilight vision. The retinal pigment epithelium, which serves as a protective layer and assists in nourishment, is found on the outer layer of retinal cells.
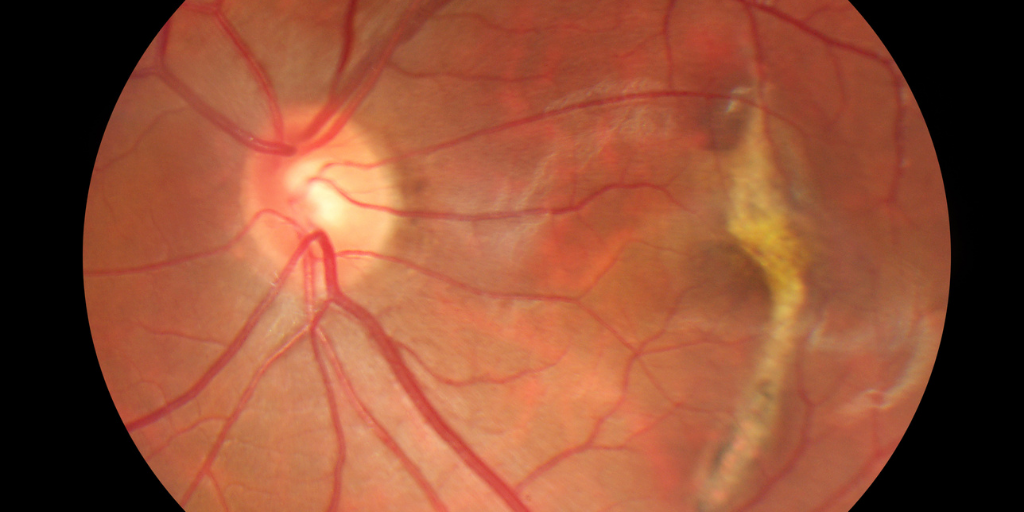
The macula, often known as the yellow spot, is a tiny portion of the retina that is involved in central vision development. Photoreceptor density is greatest in the macular region. The central fovea, which is comprised entirely of cones, is a unique depression at the very center. The key location responsible for a person’s objective vision is the central fossa.
This particular area of the retina is affected by age-related macular degeneration, which is followed by a loss of central objective vision, eventually leading to permanent blindness. The buildup of cellular breakdown products between the retina and the choroid characterizes it (vascular membrane of the eye). This mechanism is also linked to morphologically conditioned hyper and hypopigmentation of the retina at the same time. These early alterations do not yet result in degeneration and a loss of visual acuity. However, as the condition progresses, clinically significant abnormalities emerge.
A person may not notice any symptoms in the early stages of the disease, but as the condition progresses, they may feel;
Standard diagnostic methods are used to begin the evaluation (determination of visual acuity, examination of the fundus, measurement of the visual field). If distinctive alterations on the retina are detected, an extensive vision assessment is recommended, which includes the diagnostic procedures described below.
Optical coherence tomography (OCT, OST) allows noninvasively obtaining lifetime slices across the whole thickness of the retina and so assessing its structure without going into the eye cavity with any devices. The approach can detect druses, aberrant vasculature, macular edema, and other abnormalities in the retina.
Fluorescence angiography (PHAG) helps to visualize altered retinal vessels and determine which of the treatment methods will be most effective (laser coagulation, intravitreal injections, photodynamic therapy).
Perimetry is a technique that allows you to assess the state of the field of view. Since macular degeneration is characterized by a lesion of central vision, with the help of perimetry, it is possible to identify areas of visual field loss (scotomas).
The Amsler test (grid) is a simple and informative method that allows you to identify a characteristic symptom of the “wet” form of macular dystrophy – curvature of the lines. The Amsler grid has the form of thin intersecting horizontal and vertical lines. A patient with an exudative form of AMD sees the lines in the drawing as uneven, broken, or pale. The larger the area of the macula involved in the pathological process, the more distorted the lines will look when tested.
Indocyanine green angiography (ICA), like PHAGE, requires intravenous administration of a contrast agent. After a while, they take a series of consecutive photos of the retina in infrared light. This diagnostic procedure allows you to determine changes in the retina that are not detected by PHAGE.
To prevent age-related macular degeneration, it is necessary to exclude risk factors at a young age: smoking, the presence of a large amount of saturated fatty acids in the diet, excessive insolation. If risk factors could not be excluded, then after 50 years it is necessary to start preventive intake of vitamin and mineral complexes with carotenoids
The treatment of further complications is carried out either with the help of surgery or injections. However, the surgical techniques have not yet become widespread in AMD due to the high complexity and possible complications, but in some cases, that’s the key solution.
If you or a loved one has been experiencing the symptoms listed above, we recommend consulting a doctor to avoid further complications.
Take care of yourself and your family!